The aim of the group is to understand, at the molecular and cellular level, the role of human cutaneous immune responses in mechanisms of disease, treatment and vaccination. We have a particular focus on T cells which recognise inflammatory lipids presented by CD1a. As well as contributing to an understanding of disease pathogenesis, we aim to translate our findings to changes in clinical practice.

Skin frequently represents the first point of contact with pathogens and allergens, yet we still know relatively little of the role of the skin barrier and skin immune system in reacting to such challenges. This is crucially important in understanding the mechanisms of skin diseases and related diseases, and for optimising approaches to cutaneous drug and vaccine delivery.
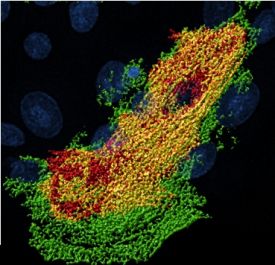
We have an ongoing interest in skin T cell responses, specifically how these can be initiated and propagated. T cells responding to peptide antigens presented by MHC molecules are well studied, but there has been less work on non-peptide antigens. We are focusing on lipid-specific CD1a-reactive T cell responses, including the involvement of phospholipase A2 (PLA2). We determined that the PLA2 enzyme can generate new lipid antigens (“neo-antigens”) in the skin and induce immune responses contributing to allergy, with important roles in atopic dermatitis (AD) and other skin diseases such as psoriasis.
We are also investigating populations of innate lymphoid cells (ILCs), which have recently been identified as a newly discovered cell type in the skin and other sites. For the past few years we have been defining the role and requirements of these cells and their cross-talk with the epidermis.
 |  |  |
|---|
Moreover, we also investigate the effect of ongoing immune responses on the epithelial component of the skin barrier. We determined that inflammatory mediators, such as cytokines and histamine, affect the integrity and function of the skin. Finally, we are interested in epidermal biology and recently helped define mechanisms governing epidermal differentiation and stratification.
We also use our findings to understand conditions which affect other organ systems; an example is dengue virus which infects 390 million people worldwide annually. We have found that some of the immunological processes we are finding in the skin, can be shared with immune responses to dengue virus.
The studies conducted within the group attempt to resolve fundamental questions related to immunology and translate these towards novel therapeutic strategies.
Collaborations
Professors Fiona Powrie and Paul Klenerman, NIHR Biomedical Research Centre
Professor Gathsaurie Malavige, University of Sri Jayawardenapura, Sri Lanka
Professor Branch Moody, Harvard University, USA
Dr Andrew McKenzie, LMB, Cambridge
Professor Padraic Fallon, Trinity College Dublin, Ireland
Professor Jamie Rossjohn, Monash University, Australia
Professor Muzlifah Haniffa, Newcastle University
Professor Tao Dong, MRC Translational Immune Discovery Unit
Funding
We are most grateful for funding support from:
NIHR Biomedical Research Centre
NIHR Clinical Research Network
Chinese Academy of Medical Sciences (CAMS) Oxford Institute (COI), University of Oxford, Oxford, UK
Public engagement
We take an active role in Public Engagement through Exhibits, School talks, public talks, blogs and podcasts.
Clinical studies and trials
We continually translate our findings through to patients, and undertake early and late phase clinical trials with an experimental medicine focus.